October 27, 2021 (changelog)
The discussion around Covid vaccines is broken.
Most people, including the media and policymakers, unilaterally tout the benefits of vaccination. Information that fits the pro-vaccination narrative is amplified, while criticisms of vaccines are suppressed - often labeled as fringe or even misinformation - regardless of their truth. Meanwhile, many vaccine skeptics rarely bother to fact-check anything that matches their anti-vaccine narrative, and they regularly amplify things that are demonstrably false.
As a result, we now have two highly-polarized echo chambers that are both making incorrect claims, ignoring sound evidence, and applying confirmation bias to everything they read. Positions are no longer logical on either side - they’re emotional. And the truth is, this is a situation with a lot of nuance that simply isn’t being discussed that way in most circles.
Kind of like this:
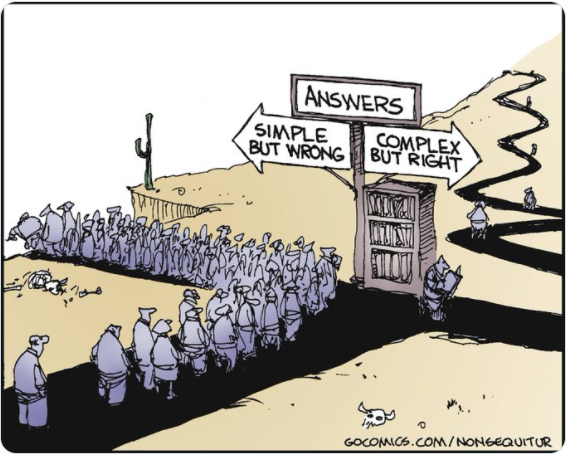
Source: Non Sequitur
In this essay, I invite you to take the path on the right with me. My story won’t match the narrative you’ve been seeing on TV, the newspapers, or in your censored Facebook groups. Instead it will be complicated, nuanced, and - if I do my job right - as accurate as humanly possible.
Let’s go.
The Problem
What does it mean to say “the discussion around Covid vaccines is broken”? Let’s start with two examples.
First, I’ll take what I consider to be a measured pro-vaccine position:
The vaccines are safe and effective. They are by far the best weapon we have to combat this disease, and have saved countless lives. Yes, there are some side effects, but they are mostly mild, and the serious ones are exceedingly rare. Meanwhile, Covid has killed millions of people. Widespread vaccination reduces the spread of Covid and makes everyone safer. It’s obvious that everyone - except kids and the immunocompromised - should get vaccinated. However, because of rampant misinformation online and the politicization of this issue, many people aren’t doing the right thing, and they are actively harming themselves and putting others at risk. Vaccine mandates should be a last resort, but they do work, and given that many people seem to be unwilling to get the vaccine under any other circumstances, need to be carefully considered and rolled out where necessary.
Are you nodding? Good.
Or maybe you’re angry. Well then, let’s try on a measured anti-vaccine position:
The vaccines were produced and approved at unprecedented speed. Additionally, several of the vaccines use an experimental mRNA technology that has never been approved for use in humans until now. They are the most dangerous vaccines that have ever been widely distributed. People have died from the vaccine, many more are getting serious medical conditions, and we have zero information about their long-term safety. Plus, the vaccines are no longer even preventing people from getting Covid and - in some cases - dying. If the vaccines protect you, why does it matter what other people do? Covid is low-risk for young, healthy people who will almost all fully recover quickly regardless of their vaccination status. Mandates are the equivalent of forcing unnecessary, experimental medical treatments on society, and an infringement upon our civil liberties.
Better?
Here’s the thing - both of these positions are, for the most part, factually correct.1 What’s happening is everyone is picking the set of facts and narratives that match their perspective and using it to reach their pre-ordained conclusions.
In the rest of this essay we’ll try to get to the bottom of the discrepancy between these two positions. We’ll do it by thinking of vaccines from a cost-benefit perspective - both to an individual and to society at large. These considerations - and the information we have surrounding them - are a complicated, imperfect mess, but we’ll do the best we can.
This essay doesn’t tackle the question of vaccine mandates head-on, but it will at least point out some places where policies are inconsistent with the evidence, and say a few things about what an evidence-based mandate policy might look like.
Ultimately, I hope this essay helps move everyone a bit towards the middle. I’ve seen families, workplaces, and communities torn apart by this issue. And I hope putting this information together might play some small part in bringing them back together.
Note: below is a summary of the conclusions of this document, followed by the complete analysis. You might initially find some of the statements presented below surprising, but all information and analysis are backed up by references and data which are cited in the complete narrative. Please bear with me, and if you feel I’ve gotten anything wrong, let me know and I will correct it!
Summary
In one line: Most people should probably choose to get vaccinated, and there are problems with how we are currently coercing them to.
In a few paragraphs:
From the perspective of an individual’s health
Based on the information we have today, if you haven’t had Covid yet, the vaccine will make you ~90% less likely to end up in the hospital and is unlikely to harm you. For most, the cost/benefit analysis of vaccines vs Covid leans heavily in favor of vaccines.
However, for some individuals - particularly those who have already had Covid, or those who are young and healthy - Covid is also exceedingly low risk. For these people, the cost-benefit analysis for vaccines - which do have rare but serious side effects - is less clear. For these groups, it is at least plausible that vaccines do more harm than good.
For others it’s a spectrum. For healthy, younger adults, Covid has real - but still low - risk. In this age range, the benefit from vaccines - in absolute terms - is still low. But the risk from vaccines is even lower. So the main reason to get vaccinated would be based on speculation that the risk from vaccines is greater than is currently understood. Some people in this category - especially those with a pre-existing distrust of the medical establishment - might choose to take the risk of contracting Covid without protection over vaccination. This decision is not supported by the current data, but is not wildly irrational. It could be compared to choosing not to get a seasonal flu shot, but with higher stakes.
The older or more vulnerable you are, the less defensible the choice not to vaccinate becomes. For those over 65 or with other health issues, vaccination appears far more likely to save your life than harm you. People in this group should almost certainly choose to get vaccinated.
From the perspective of an individual’s risk to society
Vaccines help greatly to slow the spread of Covid but are no longer effective enough to stop it. It appears that Covid will be with us forever, and likely that everyone will contract it sometime in their lifetime. Covid prevention is no longer possible, and our focus should move to Covid mitigation.
The key to Covid mitigation is 1) to prevent health systems from getting strained and 2) to minimize severe outcomes from the disease. Vaccines help a lot with both these things, by reducing the spread of disease and significantly reducing severe outcomes. Choosing to get vaccinated reduces your contribution to Covid’s toll on society and is a beneficial act.
At the same time, policies that mandate vaccines, or require regular testing for only unvaccinated people, are not logically consistent with the difference in societal risk from the two groups. The latest data on current vaccines indicate they are ~50-60% effective at stopping the spread of the disease, meaning that the unvaccinated are about twice as likely to spread Covid as the vaccinated. This is a big improvement, but it still means that a dinner party of 4 vaccinated and 2 unvaccinated people is just as risky as one with 8 fully-vaccinated people. The relative risk between these groups is not reflected by current policies, which typically draw a hard line between them - often allowing nearly unlimited vaccinated people to gather with zero unvaccinated, or requiring unvaccinated people to test regularly and vaccinated people to never test.
Finally, policies and conversations which exclude previously-infected people - who appear to have as-good, if not stronger and longer-lasting immunity than the vaccinated - are inconsistent with their risk to society.
The full cost/benefit analysis
As with any medical intervention, the core of the decision to vaccinate is a cost-benefit analysis: does the benefit provided by the vaccines outweigh the cost of getting one?
There are two components to the cost/benefit analysis: personal protection and societal protection. Personal protection applies to your own health as an individual. Societal protection applies to your contribution to the spread of the disease.
So really there are four variables to consider when making the call to vaccinate:
- Personal benefit of getting vaccinated
- Personal cost of getting vaccinated
- Societal benefit of you getting vaccinated
- Societal cost of you getting vaccinated
One hypothesis is that much of the debate surrounding vaccines is linked to different going-in positions around what the true values of the above four variables are. So the first undertaking is to try and get some data-backed alignment on those questions.
We’ll address these in the order of complexity.
The societal cost of vaccination rounds to zero
The easiest one to cover is the societal cost of getting vaccinated. That is, how much harm are you doing to society by choosing to get vaccinated?
All but the most extreme anti-vaxxers would agree that this is at or near zero.2 That is, the decision to get vaccinated does not harm society.3
Economically there is a small cost. Namely, the cost of the vaccine itself - maybe $30-50 depending on the vaccine and where you live4 - plus the cost of the infrastructure to deliver it to you - maybe another $50-100.5
The personal benefit of vaccination varies greatly
Of the remaining variables, the easiest one to discuss is personal benefit, since vaccine efficacy has been carefully studied.
In this section we’ll ignore the question of how getting vaccinated changes your likelihood of passing Covid on to others (a societal benefit) and focus exclusively on the impact they have on you as an individual.
The primary personal benefits of vaccination are:
- A reduced likelihood of contracting Covid.
- A reduced likelihood of getting very sick if you do contract Covid.
We can kind of lump them together, though, since from a personal perspective it doesn’t really matter if you catch a mild case - you’re mostly worried about avoiding severe sickness.6
So how much do vaccines help you from getting seriously sick?
The exact numbers are difficult to know with certainty since it’s a constantly evolving picture that depends on the variant, the vaccine, when you got it, etc. but the latest data from several large population studies indicate that vaccines provide a ~90% reduction in severe cases (e.g. hospitalization and death).7
If you’re vaccinated you’re about 10 times less likely to get hospitalized or die of Covid as someone similar who hasn’t been vaccinated.
So why say this varies greatly?
Because your going-in risk of having a serious outcome from Covid depends greatly on who you are.
How dangerous is Covid?
Your risk from Covid depends tremendously on who you are. There are at least three important factors in assessing Covid risk:
- A previous Covid infection
- Age
- Other health problems (comorbidities)
This section focuses mostly on death outcomes, because they have the best data, but it’s worth noting that there are other severe negative outcomes, e.g. severe injury and long Covid. Unfortunately, the data on these is difficult to find, so it’s harder to factor them in. But it seems safe to assume they have the same overall shape as the death distribution.
Previous infections
For an unvaccinated person, the most important variable in assessing Covid risk is whether you’ve already had Covid. The latest data shows that a previous Covid infection provides at least as strong immunity as vaccination, and likely stronger and longer-lasting.8 If you’ve already had Covid you are already more protected than a vaccinated person who has not had Covid and your risk from reinfection is exceedingly low. Thus the benefit of the vaccine is also exceedingly low.
Age
The next-most important risk factor is age. Most people know that Covid is far more dangerous the older you are, but many aren’t aware of just how big the differences are.
The numbers below are taken directly from the US CDC. Two quick notes about the data before diving into the analysis:
- The data spans January 2020-September 2021, likely the “worst” period of the pandemic. These numbers will probably all go down moving forwards.
- The US has the worst Covid mortality rate in the world, so these numbers are all higher than the global averages.
Ok, onto the numbers. Broken down by age:
-
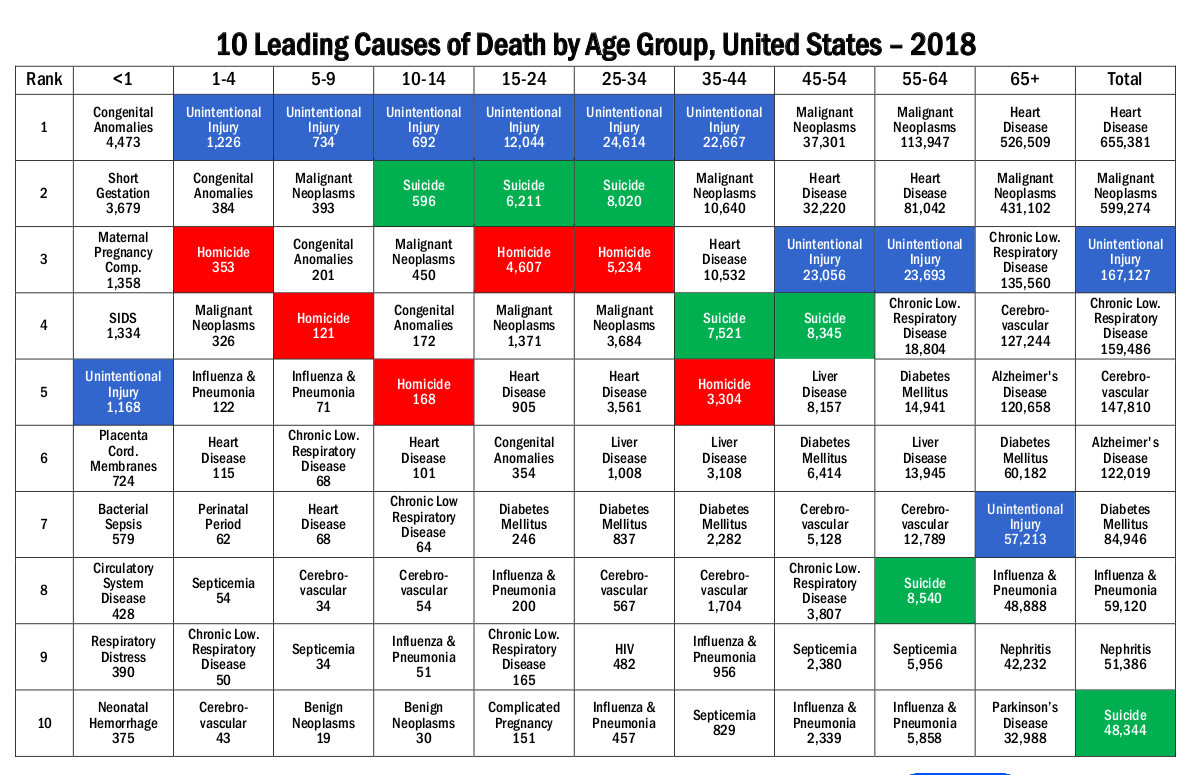
If you’re under 15, Covid is comparable to the flu (maybe 1.5x more fatal). As of September 2021, fewer than 300 people under 15 have died of Covid in the US. This represents 1 of every 175 deaths of under 15s since Jan 2020.9 However, since young people rarely die this risk is 1 in 230,000 people in absolute terms. People in this age range were about 16 times more likely to die from “unintentional injury” than Covid in the last 18 months.
-
If you’re 15-45 Covid is far worse. About 1 in 20 deaths in this range were attributable to Covid, or ~1 of every 6800 people in absolute terms. For this group, Covid deaths happened at around the same likelihood as suicides.
-
It goes up from there, and fast. At 65+, 1 in 9ish deaths were from Covid. One of every 100 people over 65 died from covid in the last 18 months (1/13 people in this age range died of all causes). This makes Covid about as deadly as heart disease, the leading cause of death in this age range.
If you assume the 90% efficacy applies across age groups then being vaccinated as a 14-year-old would have reduced your risk of dying in the last 18 months from 1/230,000 to 1/2.3 million. Likewise, a 30-year-old’s risk would be reduced from 1/6800 to 1/68,000, and an 80-year-old’s from 1/100 to 1/1000.
In absolute terms, the relative differences among these numbers is huge. You only need to vaccinate one hundred 80-year olds to save a life. For kids, that number is 230 thousand. If Vermont were made up entirely of kids and you vaccinated every person in the state you might save 2 or 3 lives.
Comorbidities
Many other factors also affect risk substantially. Obesity, other illnesses, etc. In general, healthy people tend to have milder Covid cases, so if you’re healthy you should expect to do better than the above. For example, more than 15% of COVID deaths in the US were among diabetics. The numbers get fuzzy quickly and are hard to estimate, but the CDC has a table summarizing some.
Summary
Covid is a very dangerous disease for many people, and for these people, vaccines provide a huge benefit of making them far less likely to get very sick or die. But Covid is also not very dangerous for many people, and for those people vaccines have a much smaller benefit. For children and those who have been previously infected, the personal benefit is exceedingly low.
The personal cost of vaccines is low, though not fully understood
Now we get into really difficult territory. What’s the personal cost of getting vaccinated? That is - how likely is a vaccine to harm you?
First, let’s ignore the cost from mild side effects. Your arm might flare up, you might have a fever for a few days, etc. These are annoying but - much like a mild bout of Covid - the cost rounds to zero.
The true cost of vaccines comes from severe or long-term side effects: for example, myocarditis and other heart problems, blood clots, and, of course, death.
So how dangerous are the vaccines?
This is a very difficult question to answer, because we just don’t have great data on the topic. Vaccine trials did not show any substantial risks, though they weren’t large enough to catch rarer events - those that only occur in 1 of every 5,000-10,000 people or more. This puts an upper bound on how likely these things are.
To catch rarer events we turn to VAERS.
CDC’s VAERS DB is a record of vaccine side effects (also known as adverse events) that’s designed to help find problems that might not get caught through other means. But it has several issues that make it difficult to rely on.
The first is that it reports association only. A person got the vaccine and then got sick. It doesn’t - and can’t - say whether or not the vaccine caused the sickness. People in the pro-vaccine camp are likely to believe the overwhelming majority of reports in VAERS are just a coincidence.
The second problem is that reporting is voluntary. Doctors are given guidance to report all vaccine adverse events to the system, but there is no enforcement of that guideline. Plus, doctors may not even know if a patient has an adverse reaction. As a result, most anti-vaxxers believe VAERS is underreporting the harm done by vaccines, possibly substantially.
The third problem is that VAERS is not gated. That is, you don’t need to be a medical professional to put your information in. This means that people who wanted to show that vaccines are harmful could enter fake reports into the system - something that some pro-vaccine people believe is happening.
So it’s a mess. But it’s one of the best and only messes we have to try and answer this question. And given that it’s impossible to say whether it’s over or under-counting, and that there is no evidence of over or under-reporting, we’ll just take the numbers in VAERS at face value.
Like our analysis of Covid, the easiest place to start is death, because it’s the clearest thing to measure and compare. So if you believe the numbers in VAERS, how likely is a vaccine to kill you?
The answer is “not likely”. But it might not be quite as rare as you’d expect. As of October 1, 2021, VAERS reports 16,310 deaths associated with Covid vaccines among about 400 million vaccines given over the same time period. This works out to one death per every 25,000 shots / 12,000 two-shot regimens. This puts the death rate of a single shot around the same as the rate of dying during childbirth in the US. It’s also about the same likelihood of having died from Covid in the last 18 months if you’re aged 15-45.
That said, VAERS deaths also skew towards older people. Not as dramatically as Covid deaths, but substantially. This is one reason some people think the numbers in VAERS are inflated. Because old people die more regularly than young ones. Either way, vaccines are statistically safer than that for young people - and substantially safer than Covid.
Other side effects are even harder to measure. The manufacturers acknowledge that the vaccines are associated with an increase in serious issues, including blood clots, myocarditis, and bell’s palsy. But that these outcomes are “rare”.
Myocarditis - a potentially serious inflammation of the heart - is a concerning side effect with emerging information. It now looks like the likelihood of myocarditis among certain groups - especially young males - could be as high as one in 6 or 7,000.10 This risk is causing some countries to rethink their recommendations for vaccines. In early October, Sweden and Finland suspended Moderna vaccines for those under 30, and Norway did the same for those under 18.11 Although both the Pfizer and Moderna mRNA vaccines have some myocarditis risk, the risk from Moderna may be higher. Some other countries are only recommending one mRNA dose for younger people, for example, 12-15-year-olds in the UK.12
Beyond these “obvious” side-effects, the risk from the vaccine becomes even more difficult to quantify. Because they were only developed in the last two years, it is impossible to have any long-term information about the safety of these vaccines. At the same time, it would be extremely unusual for any significant side-effects to show up years after giving the shots. So it seems highly likely that no major issues would emerge that we don’t already know about.
Another big unknown is the degree to which boosters could have additive negative effects. We know that myocarditis risk substantially increases between the first and second dose. What does that mean for the third - and maybe down the line - fourth and fifth doses? The short answer is that we have no idea. So far the third dose looks as safe as the first two - but it hasn’t been widely distributed. We’ll find out over time.
So there’s a lot of uncertainty. But at the same time, the best we can do is make informed decisions with the information that we have today. And based on the information we have, the vaccines appear to be pretty safe. Certainly safer than Covid for most adult age groups - except maybe those who’ve already had the disease.
The societal benefit of vaccines is high, though overstated
Finally we come to the most difficult question. How much does an individual getting vaccinated benefit society?
There are two main societal benefits of vaccination.
- Vaccinated people - because they generally get less sick - put less cost/pressure on our health systems.
- Vaccinated people - because they are less likely to spread the disease - transmit it to fewer people, resulting in less overall disease in the population.
We’ll start with the first one, because it’s easier to reason with.
The societal impact of getting less sick
As we saw above, individuals who are vaccinated are ~90% less likely to have severe cases of the disease. We discussed this benefit in the “personal benefit” section, but it also has societal effects. On average, vaccinated people are less likely to take hospital beds from others, will incur fewer medical costs, and will generally put less pressure on health care systems and workers.
It’s hard to quantify this cost - especially because the cost is much higher if a health system is already strained. Taking up a hospital bed when the hospital is empty is quite different from taking it up when the hospital is full and someone else is denied care.
And even if you ignore strained health systems and tired doctors, the unvaccinated people who get sicker than they otherwise would have still need to be treated, which costs money. Some studies estimate that the unvaccinated have already cost society billions of dollars in medical expenses.13
That said, it’s worth re-emphasizing that the shape of this contribution will follow the same shape as the “covid risk” section above. That is, these costs are likely to be highly concentrated among the older/sicker population, and much less common among young/healthy people or those who have already been infected. For groups like the Covid-recovered and under-18s the societal impact of getting less sick is still near-zero.
The societal impact of spreading less disease
We finally come to the trickiest topic. The one that is used to make the strongest case for mandates, the one that causes people to shame and cut ties with the unvaccinated, and the one that is the subject of tremendous debate and conflict in society.
How much does not getting vaccinated contribute to the ongoing spread of the disease?
In broad strokes, this benefit of vaccines is simple to understand:
- Vaccines reduce the likelihood of contracting and transmitting Covid.
- The less Covid is transmitted, the less damage will be done.
To start, we’ll just focus on individuals’ likelihood of getting infected and transmitting the disease to others before talking more about “herd immunity”. To proceed with this analysis we first need to know how effective vaccines are at stopping the spread of disease.
How effective are vaccines against the spread?
Initially vaccines were highly effective at preventing infection, illness and death. More recently, they have lost substantial effectiveness against infection, though are still quite protective against severe outcomes. It’s not fully known whether this reduction in efficacy is a factor of waning immunity over time or the increased virulence of the delta variant - likely some combination of both.
Either way, the latest data from CDC in the US and Isreal suggests the mRNA vaccines14 have about a 50-60% effectiveness at preventing infection against delta. They are still 80-90% effective against severe illness / hospitalization - but you’re only about half as likely to catch a breakthrough infection after being vaccinated.15
Another question is whether infected vaccinated people spread the disease as much as infected unvaccinated people. The answer appears to be “yes". After the Provincetown outbreak was analyzed, CDC confirmed “both [vaccinated and unvaccinated] groups carried equal viral loads and were equally likely to pass on their infections”16 - though there’s some evidence the vaccinated may be contagious for a shorter duration.
Boosters - when rolled out as they have been in Israel and now the US - may change these numbers. So far, boosters appear to provide strong, renewed short-term protection though their long term impact on efficacy is not yet known. There’s also not currently any reason to believe they’ll last longer than the first two doses, which means maintaining this effectiveness would require re-boosting the population every 6-8 months.
Bottom line**, based on the latest evidence, vaccinated people spread Covid a bit less than half as much as unvaccinated.**
How effective is natural immunity?
One strangely ignored factor in the vaccination discussion is natural immunity from a previous Covid infection. We know getting Covid confers some protection, but how does that compare to a vaccine?
Again, based on the latest data we have, natural immunity appears to be better than vaccine immunity. It is equally effective and longer-lasting (based on the emerging waning effectiveness of vaccines over time / against delta).17
One study “demonstrated that natural immunity confers longer lasting and stronger protection against infection, symptomatic disease and hospitalization caused by the Delta variant of SARS-CoV-2, compared to the BNT162b2 two-dose vaccine-induced immunity.”18 Several other analyses have mirrored this result,19 20 which also has a sound basis in biology.21
Natural immunity plus vaccination is the most effective, but the increased benefit on top of the already-highly-effective natural immunity is very small. Plus, people who have already had Covid are also more likely to have side effects from the vaccines.22
Either way, naturally immune people catch and spread Covid far less than vaccinated people who haven’t been infected. This is a place where many vaccine policies and mandates - which often ignore natural immunity - are wildly out of line with the evidence of those people’s societal risk.
How fast does Covid spread?
Based on the above, we can first say two things:
- Vaccinating people who haven’t had Covid makes them half as likely to spread the disease.
- Vaccinating people who have had Covid provides a negligible benefit.
That’s at an individual level. But these impacts are based on a population. Disease spreads exponentially through a population and reducing the exponent can be a big deal.
One way to model disease spread is through the R0, or R-naught, number, which represents the average number of people an infected person will spread the disease to. If R0 is below 1 - meaning that each infected person infects less than one other person - the disease fizzles out quickly. Conversely, if R0 is above one, the disease spreads through a population infecting more and more people. The higher the R0, the faster the disease spreads.
R0 is difficult to measure, because the spread of disease is impacted by the amount of immunity in the population (through vaccination or previous infection) and on behavior. Masks, social distancing, and lockdowns all serve to reduce the R0 of a disease.
Still, scientists try to estimate the R0 of diseases, typically assuming a non-immune population acting “normally”. So what’s the R0 of Covid? The CDC estimated the R0 of delta to be between 5 and 9 among an unvaccinated population.23 Let’s assume a relatively conservative number of 6.
If the R0 is 6 among the unvaccinated, then it’s between 2 and 3 among the vaccinated - well above the threshold that would prevent the disease from spreading. Covid will spread through vaccinated and unvaccinated populations alike, unless other measures (e.g. masking, distancing) are introduced. It will spread faster among the unvaccinated, but based on our current vaccines we can’t stop this disease from spreading until the overwhelming majority have caught it.
Unless something big changes - e.g. we get better vaccines - most people will meet this virus eventually.
Protecting your friends and family
R-naughts help us understand how disease spreads through a population, but they don’t really capture what it feels like to pass Covid onto someone. The nightmare scenario is transmitting Covid to someone who then goes on to have a severe outcome. No one wants Grandma’s death on their shoulders.
Here the case is pretty clear: if you want to do everything in your power to minimize your contribution to negative outcomes, get vaccinated.
That said, vaccines are not the only tool we have to protect our loved ones. Going for a walk in a park with an unvaccinated person is statistically far safer than having dinner indoors with a vaccinated one. Vaccines are one pillar of disease prevention, and if you choose not to get one, you should try and compensate with other ones - e.g. masking, distancing, avoiding crowds, etc. These should be employed in proportion to the absolute risk you’re willing to put on those around you. But you should be very aware that in the absence of any other behavior changes, not getting vaccinated does make you twice as likely to kill a loved one. You’ve been warned.
What does all this mean for policy?
Based on the above we can find some inconsistencies in our current policies when viewed from a public health perspective.24
First, all policies should account for natural immunity. In many places, including basically the entire US, having previously had Covid does not “count” towards Covid restrictions, despite that fact that previously infected people are safer to society than vaccinated people who’ve never had Covid.
Second, our testing rules are highly illogical. Remember 50% efficacy means that unvaccinated are ~2x likely to contact Covid as vaccinated. Yet, many mandates propose that the unvaccinated be subject to weekly tests, while vaccinated require no testing. This is just bizarre logic that does not make statistical sense. In a society where half the people were vaccinated and half were unvaccinated, ⅓ of the cases will come from the vaccinated group. But you don’t test them at all?
Third, policies should adapt based on the baseline rate of disease. By far, the most important number to assess the absolute risk of catching Covid is the number of other people around you who have it. If a wave of Covid is running through a region - let’s say 1% of the population is infected - and restaurants decide to only let in vaccinated people, that’s a perfectly reasonable decision. But if the wave passes and suddenly only .1% of the population has Covid - then letting in 100% unvaccinated people is still far safer than what they were doing during the peak. Unfortunately, very few of the policies being put in place are taking “background Covid rate” into account at all.
Conclusion
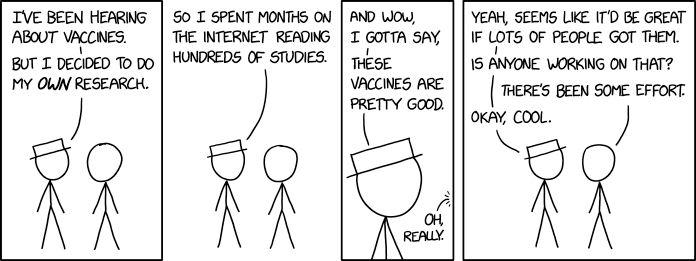
Source xkcd
This document doesn’t totally disagree with the above, though it’s oversimplified.
By and large, if you haven’t had Covid and you’re an adult you should probably choose to get vaccinated. A vaccine might save your life, is unlikely to injure you, and reduces the overall burden on health systems.
But, if you are healthy, not old, and don’t want to get vaccinated, that’s also an acceptable choice. You are taking on increased risk to your health and the health of those around you, but you’re also an adult capable of making those decisions.
Society mandating vaccines is an overreach and current policies are in no way aligned with the data we have. At an absolute minimum, any mandates should treat a previous Covid infection comparably to a vaccine. Additionally, other restrictions should accurately reflect that vaccinated are only about 2x safer than unvaccinated, but not immune to catching Covid. Restrictions should be adjusted relative to baseline Covid rates.
Acknowledgements
Thanks to the doctors, big pharma employees, and vaccine skeptics who reviewed early drafts of this essay. I know that none of you agree with everything written above, but your feedback was critical in pointing out where there were problems, and helped make the essay stronger and more balanced.
I started working on this essay because I thought I was the only person who had a centrist, evidence-based take on Covid and vaccines. However, during the research process, I found a small number of kindred spirits doing great work in this area. Their ideas and analysis helped greatly towards formulating my own opinion.
Dr. Vinay Prasad (Twitter, YouTube) has been consistently weighing the pros and cons of vaccines at the individual level. His YouTube channel is a consistent place to find highly-informed and nuanced reactions to the latest developments related to the pandemic. His podcast with Bari Weiss speaking to vaccine skeptics is a good introduction to his philosophy.
Professor Jeffrey S. Morris (Twitter) is a data scientist who runs the excellent Covid Data Science site, providing “reporting and balanced evaluation of research results, data sets, applications and models, and commentaries related to Covid-19 and its underlying virus, SARS-Cov-2”. He has done a great job both supporting some “controversial” positions such as the overwhelming evidence for natural immunity as well as refuting claims made by prominent anti-vaccine people about vaccine safety.
Aaron Kheriaty, MD (Twitter, Substack) is the Director of Medical Ethics at UC Irvine. He refused to comply with his University's vaccine mandate, citing natural immunity and an “ethical responsibility”, and is now engaged in a legal battle for his career. He beats the drum on the evidence supporting natural immunity, and is quick to point out where policies and evidence are not aligned.
References
This section provides references and further context on some of the numbers and information quoted above.
On Vaccine Effectiveness
The 50-60% number for vaccine effectiveness against infection against Delta several months after receiving the vaccine comes from several places.
One source of this figure - which was referenced in the New York Times in August - was a population study published by the CDC of over 10 million people. The relevant data can be found at the chart in the bottom, which is reproduced below.
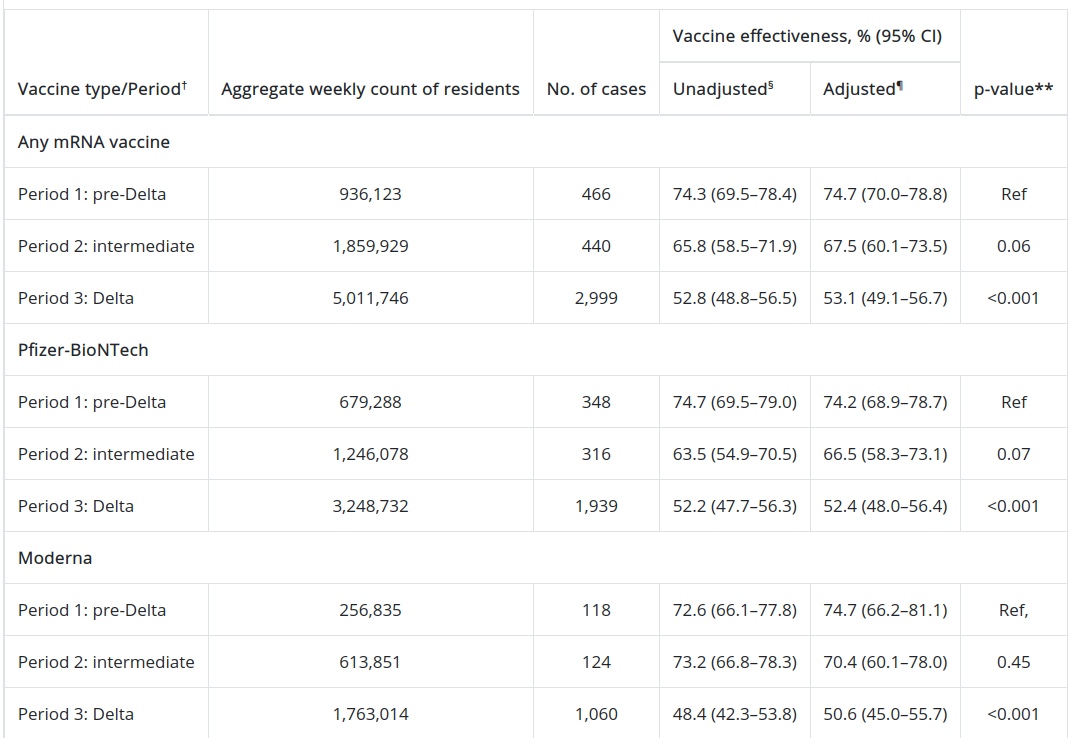
Similar conclusions have been reached from analysis of Israel data, Qatar data, and other US-based populations.
Several studies quote a higher number, closer to 70% for symptomatic infections. But because asymptomatic people can still spread the disease this number does not reflect societal protection.
The 80-90% number for vaccine effectiveness against hospitalization and death has been widely recognized in many studies - notably from Israel. Also, the difference between 80% and 99% is not particularly relevant to any position in this doc. What’s far more important is your baseline Covid risk.
On Covid mortality
All data on Covid mortality by age comes directly from the CDC’s “Provisional COVID-19 Deaths by Sex and Age” dataset. The numbers used in this essay were pulled in September of 2021, though have not demonstrably changed. A summary table can be found below:

On all-cause mortality
All references to all-cause mortality come directly from the CDC’s “Leading Causes of Death and Injury” page. The numbers used were from 2018, and are summarized in the below graphic.
On natural immunity
The evidence for natural immunity being as good as - and likely better than - vaccination alone, is overwhelming.
The Brownstone Institute has compiled a list of references on this topic that includes 30 academic studies, as well as several media references.
Some of the most compelling narratives from reputable sources include “Having SARS-CoV-2 once confers much greater immunity than a vaccine—but vaccination remains vital” from Science, and “Vaccinating people who have had covid-19: why doesn’t natural immunity count in the US?” from the BMJ.
Changelog
This essay is a living document. It will be updated as new science emerges and flaws are pointed out. My hope is to make it the best summary of this topic.
The changelog below serves as a record of how the essay has changed over time.
October 27, 2021: Added “Acknowledgements” section. Minor editorial corrections.
October 15, 2021: Initial publication.
Notes
- They both draw subjective conclusions based on the presented facts, but facts themselves aren’t wrong.↩
- Some anti-vaxxers are worried about things like “spike protein shedding” from vaccinated people, but there isn’t any credible science to back this position.↩
- A plausible “societal harm” position might argue that a young, healthy person getting a vaccine before a higher-risk old, frail person is a form of harm, but this is mostly a sequencing thing and out of scope for the purposes of this document.↩
- Covid-19: Countries are learning what others paid for vaccines↩
- This number is difficult to estimate, but you can get a decent proxy by finding a government’s total COVID vaccine budget dividing it by the eligible population and subtracting the cost of the vaccine itself.↩
- From a societal perspective, catching it matters much more, but we’ll cover this later.↩
- Citations from CDC and Isreal government later in the doc.↩
- Citations for this appear in the "On natural immunity" section of the references.↩
- All data from CDC, screenshotted and linked in references section.↩
- Myocarditis after BNT162b2 mRNA Vaccine against Covid-19 in Israel | NEJM↩
- Covid-19: Sweden, Norway, and Finland suspend use of Moderna vaccine in young people “as a precaution”↩
- Coronavirus (COVID-19) vaccine for children aged 12 to 15↩
- Unvaccinated COVID-19 hospitalizations cost billions of dollars↩
- Pfizer only, in the case of Israel.↩
- Here is the CDC analysis of mRNA vaccines and delta. Here’s a forbes article linking to the Isreal data with similar findings. Many previous studies estimated this number to be higher, but most are based on out-of-date data, or populations who have had the vaccine more recently.↩
- Discussion in BMJ here.↩
- In the absence of boosters.↩
- Comparing SARS-CoV-2 natural immunity to vaccine-induced immunity: reinfections versus breakthrough infections↩
- Overwhelming evidence now that previously infected have robust immune protection against reinfection↩
- Naturally enhanced neutralizing breadth against SARS-CoV-2 one year after infection↩
- Basically, that vaccines target only the spike protein, whereas natural immunity allows your body to produce a blended approach against all aspects of the virus.↩
- Vaccine side-effects and SARS-CoV-2 infection after vaccination in users of the COVID Symptom Study app in the UK: a prospective observational study↩
- Delta Has Changed the Pandemic Endgame↩
- If the only goal of a policy is to increase vaccination rates, then they are consistent. However, vaccination rates and public health outcomes - though related - are not the same thing.↩